Immunomodulatory properties of stem cells from human exfoliated deciduous teeth
Human bone marrow mesenchymal stem cells
(BMMSCs) have been identified as a population of
postnatal stem cells with the potential to self-renew and
differentiate into osteoblasts, chondrocytes, adipocytes,
and neural cells [1-5]. BMMSCs also exhibit immunomodulatory
and regulatory effects on T and B lymphocytes,
dendritic cells, and natural killer cells, indicating
an attractive feature for cell therapy [6-11]. In addition,
culture expanded BMMSCs may fail to express MHC-
class II antigens on their surfaces, therefore allogenic
BMMSCs have been used in treating a variety of diseases
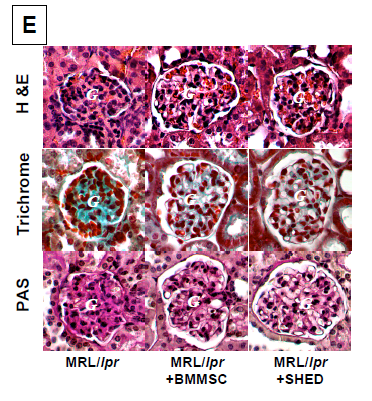
such as acute graft-versus-host-disease (GVHD) [12-14],
ameliorating
Hematopoietic Stem Cell engraftment [15,
16], and systemic lupus erythematosus (SLE) [17].
Recently, mesenchymal stem cells derived from other
tissues have also been found to possess immunomodulatory
functions [18-20] which offer opportunities
to find more effective and feasible mesenchymal stem cell
sources for cell therapies.
Stem cells from human exfoliated deciduous teeth
(SHED) have been isolated from naturally exfoliated
deciduous teeth with the capacity to differentiate into
osteogenic and odontogenic cells, adipocytes, and neural
cells [21]. As neural crest cell-associated postnatal stem
cells, SHED express a variety of neural cell markers
including nestin, beta III tubulin, GAD, NeuN, GFAP,
NFM, and CNPase [21]. Also, SHED are able to form
bone when transplanted in vivo [22] and offer obvious
bone regeneration for repairing calvarial defects in a
mouse model [23]. It is unknown whether SHED possess